Enterocolitis Information
Click here to scroll to the list of available medications ↓
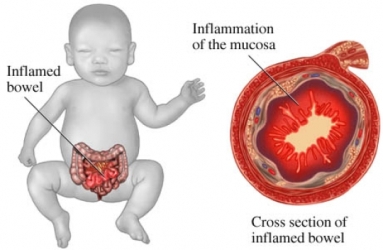
When a person's colon and small intestines become inflamed, this may very well be the start of Enterocolitis. Enterocolitis, also known as coloenteritis, occurs when the small intestine is afflicted with enteritis, and the large intestine, particularly the colon, is beset with colitis, both of which are inflammatory conditions.
There are three specific types of the disease. Necrotizing Enterocolitis occurs in infants who have been born premature. Signs of the disease will manifest themselves inversely depending how premature the infant is. A baby who has been born early will show symptoms of the disease at a later stage. Autistic Enterocolitis is a type of bowel ailment that presents similar coloenteritis symptoms typical in autistic children. Pseudomembranous Enterocolitis is a colon infection caused by a bacterium known as Clostridium difficile. Neutropenic Enterocolitis, meanwhile, is a fatal inflammatory disease with a high mortality rate that affects both the small and large bowels of patients who suffer from myelosuppression and immunosuppression.
Patients who have been diagnosed with Enterocolitis exhibit symptoms of fever; swelling in the abdomen due to inflammation of the small intestine and colon; nausea and vomiting that occurs when the inflamed intestines cause the digested food to double back upon itself, and diarrhea. The patient will also experience bleeding from the rectum, as well as a general sluggishness.
With Necrotizing Enterocolitis that afflicts premature infants, symptoms are manifested in feeding intolerance, a swollen abdomen, and bloody stools. As the disease progresses, the infant's abdomen becomes discolored due to tears in the intestines. When the infant's condition reaches this stage, emergency medical intervention is required to prevent the onset of peritonitis and hypotension.
Psuedomembranous Enterocolitis, on the other hand, is manifested by foul-smelling diarrheal expulsions, a high fever, and severe abdominal pain. These conditions can lead to toxic megacolon, an illness that is fatal if left untreated.
There are several classifications of the causes of inflammation in the small intestine and colon. Pesudomembranous Enterocolitis is a classification of the disease caused by the use of antibiotics that leads to an abnormal change in the flora found in a person's bowel. The resulting irritation and inflammation is responsible for diarrheal symptoms in patients.
Under the hemorrhagic classification, the disease is characterized by the breakdown of the mucous membranes of the intestines, resulting in hemorrhage as the cells of the intestinal walls are infiltrated due to inflammation. The Psuedomembranous classification is described by an inflammation of the bowel's mucous membranes. This inflammation is the result of pseudomembranous plaques that form as a result of antimicrobial therapy. Finally, Enterocolitis classified as ulcerative stems from infections that are bacterial and fungal in nature. These infections cause ulcers to form in the enteric mucosa.
To confirm a diagnosis for Enterocolitis, the doctor will take down the patient's complete medical history as well as subject the patient to a thorough physical examination. The patient will need to undergo a complete blood count to check for the presence of Neutropenia, and a blood culture to rule out any fungal or bacterial sepsis. Other tests may also be required, such as stool exams to rule out the possibility of Psuedomembranous colitis, and a stool culture to check for Enterocolitis caused by bacterial infections.
The doctor may also order imaging studies, such as abdominal radiographs for suspected Neutropenic Enterocolitis. From the results of the radiographs, the doctor will check for the presence of dilation in the colon or small bowel, signs of thumb printing in the right colon, a colon filled with fluid, pneumatosis, or displacement of the small bowel due to accumulation of soft tissue mass.
An abdominal ultrasound is another important test that the doctor may order. This diagnostic exam will determine whether there is any evidence of thickening in the bowel walls. In recent prognostic studies, bowel wall thickening (BWT) of more than 5mm has been pinpointed as causing a higher mortality rate.
The doctor may also require an abdominal CT scan to check for thickening in the cecum, pericecal inflammation, and an air-filled perforated or fluid-filled cecum.
While medical professionals are divided between conservative medical therapy and surgical procedures to cure patients and provide relief of symptoms, treatment for Enterocolitis will depend on the symptoms exhibited by the patient, and the extent of the disease's progress. An individual approach to each patient will be one of the doctor's first priorities in terms of medical intervention.
Conservative treatment of Enterocolitis cases include nasogastric suction and bowel rest. The doctor will observe the patient closely and conduct regular abdominal examinations under an intensive care environment. The patient will be receiving intravenous fluids, as well as blood transfusions and platelet transfusions whenever the doctor deems it necessary. To prevent the disease from worsening, no anti-diarrheal drugs or anticholinergic agents will be administered.
The patient will also be given parenteral broad-spectrum antibiotics, such as Metronidazole. Administering antibiotics to patients suffering from Enterocolitis is also done on a case-to-case basis. This is due to the probability that the patient will already have received several courses of the same type of medication to relieve the symptoms of the disease. Consequently, if further antibiotic treatment is required, the doctor may use a combination of medications, such as imipenem and amikacin, or cefepime and metronidazole, as well as vancomycin.
The antibiotics that are administered are geared at controlling and getting rid of any possible infections, whether primary or secondary, which cause sepsis within the colon and small intestine.
When patients exhibit perforated tissue in their colon or intestines, if they do not respond to conservative medical management, or if they continue to manifest intra-abdominal hemorrhaging, sepsis and formation of abscesses in the affected areas, then their only recourse would be a surgical procedure.
There are three surgical procedures recommended for grave Enterocolitis symptoms. One is a cecostomy and drainage of any accumulated fluid, air, and abscesses. Another is a two-stage procedure that involves right hemicolectomy, as well as total abdominal colectomy. The third surgical procedure is to remove the infected and inflamed portions of the colon through a loop ileostomy.