Oophorectomy Information
Click here to scroll to the list of available medications ↓
Surgery is a medical retreat to stop certain medical conditions from getting worse. There are some cases, however, where surgery becomes a reason for increased health risks. People who underwent Oophorectomy know this best.
Oophorectomy is a prophylactic surgical process that removes an ovary or ovaries from a woman’s reproductive system. This procedure is tagged prophylactic because it is intended to prevent, rather than cure, a disease. In this case, the disease we are concerned about is mostly cancer.
Oophorectomy is performed at the sight of ovarian cancer or breast cancer risks. It is basically undertaken to remove cysts or any other substance that may heighten a woman’s risk to contract cancer along with the ovary itself, the Fallopian tube or even the uterus. It is also helpful in removing the source of levels of estrogen that stimulates cancer. Oophorectomy is also sometimes used to treat endometriosis. Although rare, Oophorectomy is proven effective to prevent the thickening of the lining in the uterus.
Although parts of the woman’s reproductive system are involved in Oophorectomy, it is not similar to ligation, which is the most common form of birth control. Women who underwent Oophorectomy may still bear a child if only one ovary is removed. If both ovaries are removed, however, menstruation naturally stops along with the chances of pregnancy.
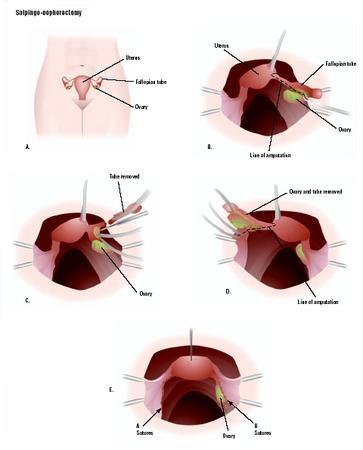
Like many surgical processes, Oophorectomy is handled under general anesthesia. The incision is similar to an abdominal hysterectomy, either horizontal or vertical, to give the surgeon a better view of the abdominal cavity. Then the affected parts are removed. Sometimes it is just an ovary or both ovaries. Other times, the fallopian tubes are also removed. In some cases, laparoscopic procedure is used to handle Oophorectomy. This way, a small incision is all that is needed to create a passage for a tiny camera lens that will help the surgeon see through the insides of the abdomen through a video monitor.
A doctor’s diagnosis confirming your risks for cancer due to ovarian cysts or tumors makes you an appropriate candidate for Oophorectomy. Women who have family histories of ovarian and breast cancers should wisely take action of preventing the fearful scene taking life by going under the knife. Before the procedure is performed, several tests are also handled to ensure that the patient is fit enough.
When Oophorectomy is intended to reduce cancer risk, both ovaries are usually removed in a process that is called Bilateral Oophorectomy. However, doctors do take considerations with young women who are yet to start their families. If it will not affect their chances for cancer recurrence, doctors may agree to perform Unilateral Oophorectomy instead and save an ovary.
During the 1980s, many cases of Oophorectomy has been performed even to women who have healthy ovaries and fallopian tubes to save them from an ovarian cancer risk that naturally rise after menopause. When the side effects of the procedure were found out during the 1990s, women start thinking twice about going through Oophorectomy unless it is badly needed. Regardless of all the risks involved, Oophorectomy remains the treatment of choice for women who fear the big C. In fact, 2004 recorded almost close to .5 million cases of Oophorectomy. Why? Because it has been found very, very effective. As a proof, patients who already carry genetic mutations of BRCA1 or BRCA2 reduce their risks for breast cancer from 80% to 19%. Although ovarian cancer is low-ranking on the fatal diseases list, it is still important to know that there is something you can do in case it becomes one of your concerns.
Going under the knife for Oophorectomy is never that easy, especially in the long run when complications start to crop up. Short-term effects include ordinary surgery risks as blood clot, internal bleeding, accidental injury to other organs, infection, and emotional trauma. Long-term effects are far more serious. Add to that is the truth that Oophorectomy does not erase the occurrence of cancer completely. In some cases, cancer has already spread in other parts of the abdomen so removal of the ovaries cannot ensure absolute freedom from the disease.
Then there is the given fact that Oophorectomy accelerates menopause. And it is not as simple as that. The hormonal change and the symptoms in this case are far more severe than when you are going through the normal menopausal cycle. All the troubles of non-production of hormones continue until the natural age of menopause takes its place.
Aside from sudden and severe menopausal symptoms, Oophorectomy also increases women’s risk for cardio-vascular diseases. The cause is not clearly known but studies showed that women who went through the surgical process of ovary removal are seven times more vulnerable to contract heart ailments later on.
Early onset of osteoporosis and other bone density problems have also been found likely to occur to Oophorectomy patients. This is also associated with sudden hormonal loss.
Sexuality dysfunction is also common among women who underwent Oophorectomy. Failure to have an orgasm and sexual desire in general are seen as probable results of going through the process. This can also happen during menopause but reduced sexual wellbeing after Oophorectomy is far greater than normal.
To manage the effects of Oophorectomy, a Hormone Replacement Therapy is prescribed. HRT has been getting criticisms since it was introduced due to established risks. But patients still choose to take hormone supplements to improve the quality of their lives and control the harsh effects of sudden hormonal loss than mind the consequences. Physicians also continue to prescribe HRT to their patients believing that the risks are nothing compared to its benefits. That does not mean, however, that hormonal therapy programs are the only way you could handle the effects of Oophorectomy. Non-hormonal programs are also available to tackle problems as bone fracture risks. Some Selective Serotonin Reuptake Inhibitors such as Prozac are also known to alleviate menopausal symptoms.
The best thing to arm yourself for braving the misery of Oophorectomy is a comprehensive information about the procedure itself. Once you find that you are a candidate for it, talk to your doctor if other options are available. If not, ask everything about Oophorectomy. Knowing what you are actually immersing yourself into prepares you best for the difficult times ahead.