Otitis Media Information
Click here to scroll to the list of available medications ↓
Otitis media is the clinical term for a middle ear infection, and they are quite common, especially in children. Typically by the age of 3 years old, a child has experienced at least one ear infection. Otitis media is less common in adults, although a middle ear infection can strike anyone.
Symptoms of a middle ear infection include fevers and ear pain. Often very young children can not explain where or why they are pain, and they may exhibit sudden changes in behaviors which include tugging, pulling, or placing fingers in their ears, excessive crying accompanied by a fever, a sudden inability to fall asleep or stay asleep, a failure to respond to sounds or directed vocal commands, experience headaches, experience fluid that drains from the ears, typically pus filled fluid that looks horrifying to a parent, and a general irritability.
Viral infections are typically the culprit of an ear infection. The ear becomes inflamed and fluid begins to develop around the middle ear. This causes pain and pressure. The fluid can build up to the point where it restricts hearing and flows from the ears, especially when lying down, before a fever develops.

The narrow passages which connect the ear to the nose can also be somewhat malformed, which causes intense and usually chronic middle ear infections in young children. Fluid in an adult’s ear is easily able to follow the tubes, known as Eustachian tubes, and drain outward. In a child’s ear, the tubes are too small and do not allow for natural draining to occur. This increases the likelihood for fluid build up and pressure, which can also fester bacteria. Chronic infections like these often lead to a procedure known as placing “tubes in the ears.”
Swelling of the adenoids can also lead to otitis media. Adenoids are located near the ear, in the upper throat which can cause infection. Swelling of the adenoids prevents draining of natural fluid in the ear, which then builds up in the middle ear, causing an infection.
Children’s immune systems are not yet fully developed and they tend to contract more viruses and bacterial infections than adults do because of their lack of immunity to everyday viruses and bacterium.
Risk factors for otitis media include especially narrow or mal-deformed Eustachian tubes, age, a poor air quality in the home such as exposure to second hand smoke, the common cold, family history, exposure to a wide variety of children such as child care facilities, race as Native American and Eskimos from Alaska tend to have a very high rate of otitis media, and feeding position. Babies who feed from a bottle in a lying position have more incidents of otitis media than babies who are held upright in a nursing position.
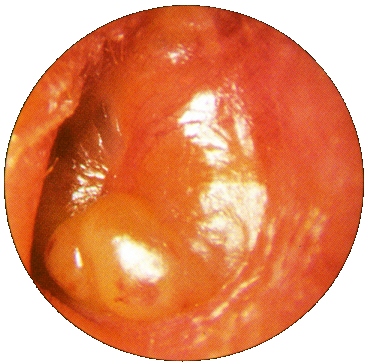
A physical examination is required to diagnose an ear infection, although once a child has had one, they can usually be sure of the diagnosis before they receive one from a physician. However, a physician is still needed to verify the diagnosis and often to prescribe treatment. Acute otitis media means there is a large amount of fluid trapped in the ear which is obvious a sign of infection. Sometimes the infection clears but leaves behind a fluid in the ear which is still painful and presents risks of re-infection. This is known as otitis media with effusion. A physician can look into the middle ear with instrumentation to view exactly what is going on inside the ear. An otoscope lights up the ear canal and allows for clear vision into the ear canal when it is straightened by gently tugging the ear downward. In severe cases, tests known as tympanometry and acoustic reflexometry are performed when a child has had a chronic case of otitis media. A tympanometry determines the movement of the eardrum and an acoustic reflexometry is used to measure the variance between empty space and fluid in the ear canal.
Undiagnosed and untreated otitis media can lead to either short term or long term hearing loss as well as the possibility of a ruptured eardrum. When treated promptly, ear infections usually don’t present much risk at all.
For children who are older than six months and have had ear infections in the past without complications, wait and see is often the first approach. At the first sign of worsening symptoms, a physician should be contacted and returned for another examination. Antibiotics may be used in very young children, children with worsening symptoms, and children with chronic or returning ear infections. Often drops to help relieve the pain and a fever reducer is recommended as well. In severe cases with chronic infections and complication risks, the child may be a candidate for drainage tubes. These tubes allow for the constant drainage of fluid until the child is older, at which time the tubes will fall out on their own and the drainage holes will independently heal.
Children are usually uncomfortable when they have ear infections, and besides relieving the pain with warm compresses, fever reducers and pain relievers, children do well in calm environments that allow them to engage in quiet and peaceful activities as well as fall asleep as their body requires.